Did you know…
Some doctors are given cash bonuses for persuading women to get screening mammograms.
One ethical doctor published a paper in the British Medical Journal, April 3, 2019:
“Our practice has recently been invited by the local clinical commissioning group to take part in a quality improvement scheme aimed at increasing the uptake of cancer screening. We are offered support from Cancer Research UK to make an action plan to improve rates of bowel, cervical, and breast cancer screening. We’re incentivised with payments for engaging in the process and for any increase in the proportion of our patients screened.”
“Dr. Salisbury is to be congratulated on her honesty. No GP should be put in this position of being rewarded for meeting targets of compliance with screening, whilst denying the patient the right of informed choice. The NHSBSP management must shoulder this responsibility by setting out the pros and cons of screening for breast cancer without making any covert coercion. As chance would have it I’m off to Lugano in two weeks to be interviewed on Swiss TV in a programme that celebrates the de-implementation of screening by mammography in Switzerland.”
More insightful responses:
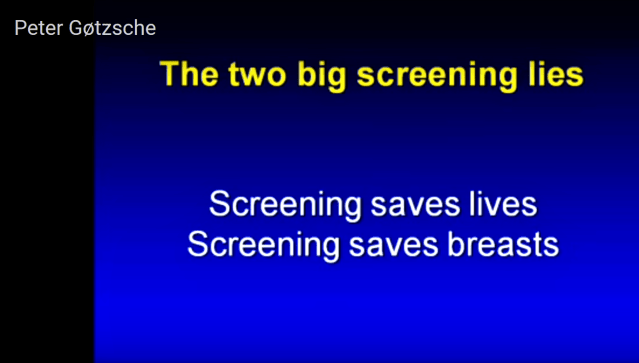
“Helen Salisbury is quite right. We do not know if the benefits of screening mammography exceed the harms. The problem is though that to the public the “catch it early” slogan is divine truth. The public does not know what “it” and “early” are. “It” may be a harmless in-situ carcinoma or benign microcalcification, and “early” may be a small tumour that has metastasized widely. Fortunes are being wasted on screening and many lives are being devastated.” – Re: Helen Salisbury: Should I persuade patients to have mammograms? The “catch it early” myth, Roger H Armour, Retired consultant surgeon
“Back in 2012, despite increasing evidence of breast screening harms and lack of benefit, GPs were being paid to encourage women to participate in the programme as part of ‘local enhanced services payments’ if a health authority deemed recruitment was getting too low. Such payments were not ethical then; in light of today’s knowledge, are they not destined to invite litigation?” – Mitzi A J Blennerhassett, medical writer/author, bmj patient reviewer
“The short answer to the title question is “No! Definitely not.”
A trusted doctor should be one who guides his/her patient to reliable information and encourages them to contribute to a well-considered shared, but individual decision that respects BOTH party`s rights to self-determination according to their own values, individual circumstances and preferences. No interference of State!
The limited consultation time is short enough anyway: it should not be used by the doctor to promote public health issues: a reversal of a true doctor-patient relationship. His/her patient will have taken the initiative to make the appointment and should be free to raise those issues which concern them, without imposition of public health promotion. Especially where the conscience of the doctor is troubled, both by being offered a payment to raise a Public Health Authority issue that is directed at citizens, not patients, and especially when they are uncertain of the value of the intervention – in this case the harm benefit ratio of breast screening? The power of Public Health to blackmail by payment incentive and override the judgement of individual doctors is insidiously corrupting the Profession, crushing its judgement and professionalism, as Seamus O`Mahony has so eloquently written about. Overdiagnosis with resultant wastage of resources stem from this reversal; a sad consequence of this uncalled for activity.” – Hazel Thornton, Honorary Visiting Fellow, Department of Health Sciences, University of Leicester
Thank you Dr. Salsbury and all who wrote responses.
For more responses to Dr. Helen Salsbury’s BMJ article, see rapid responses







 The percentage of women who need a 2nd or 3rd surgery after a lumpectomy, (also called breast conserving surgery (BCS) or partial mastectomy) is alarmingly high — especially for DCIS (stage ZERO breast cancer). One study showed
The percentage of women who need a 2nd or 3rd surgery after a lumpectomy, (also called breast conserving surgery (BCS) or partial mastectomy) is alarmingly high — especially for DCIS (stage ZERO breast cancer). One study showed 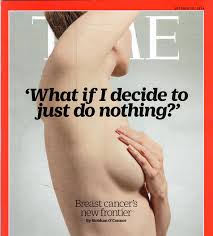 I did not “do nothing.”
I did not “do nothing.”
