I think we can all agree, when it comes to our health, we would prefer clear information on risks and benefits vs being oversold.

But, when it comes to mammograms, most women do not even realize they have NOT been given informed consent. Many say they feel encouraged, pressured, and even coerced into scheduling a screening mammogram. There is often no mention of risks or harms. Not from doctors, not from breast cancer charities, not from celebrities, and not from the media.
Unfortunately credible resources and good scientific information have been drowned out with marketing slogans.
“Get Your Mammogram! Early Detection Saves Lives.” These messages are heard over and over, but is this doing more harm than good?

This blog post aims to provide women with actual facts and clear information which help provide informed consent to women about mammography screening.
What is Informed consent?
The short definition: “Informed consent is the process in which a health care provider educates a patient about the risks, benefits, and alternatives of a given procedure or intervention. (See longer definition below).
Another issue which overshadows informed consent are all the arguments about various guidelines. When to start, when to stop, how often, and now there is emphasis on newer technology such as 3D or contrast enhanced mammograms. There is even some discussion about dense breast tissue. But women are often still unclear on what to do if they have dense breast tissue.
Examples of Clear Information, Not Marketing
The Harding Center for Risk Literacy created “fact boxes” to illustrate benefits and harms of early detection of breast cancer by mammography screening.
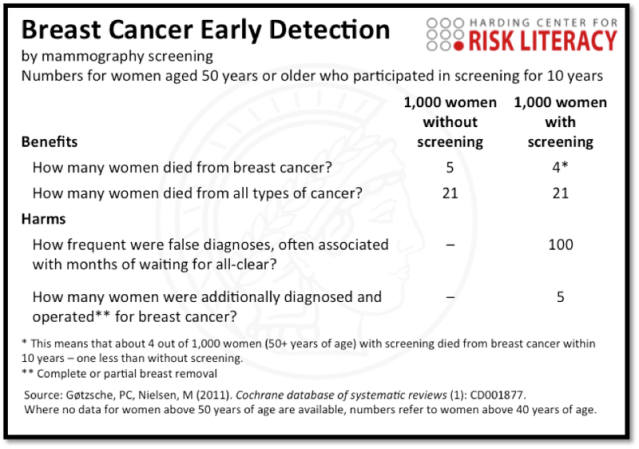

Summary: One life saved out of 1,000 women screened, but 5 lives harmed.
Another chart shows estimates of benefits and harms of annual mammography screening over 10 years of 10,000 women in their 50s:
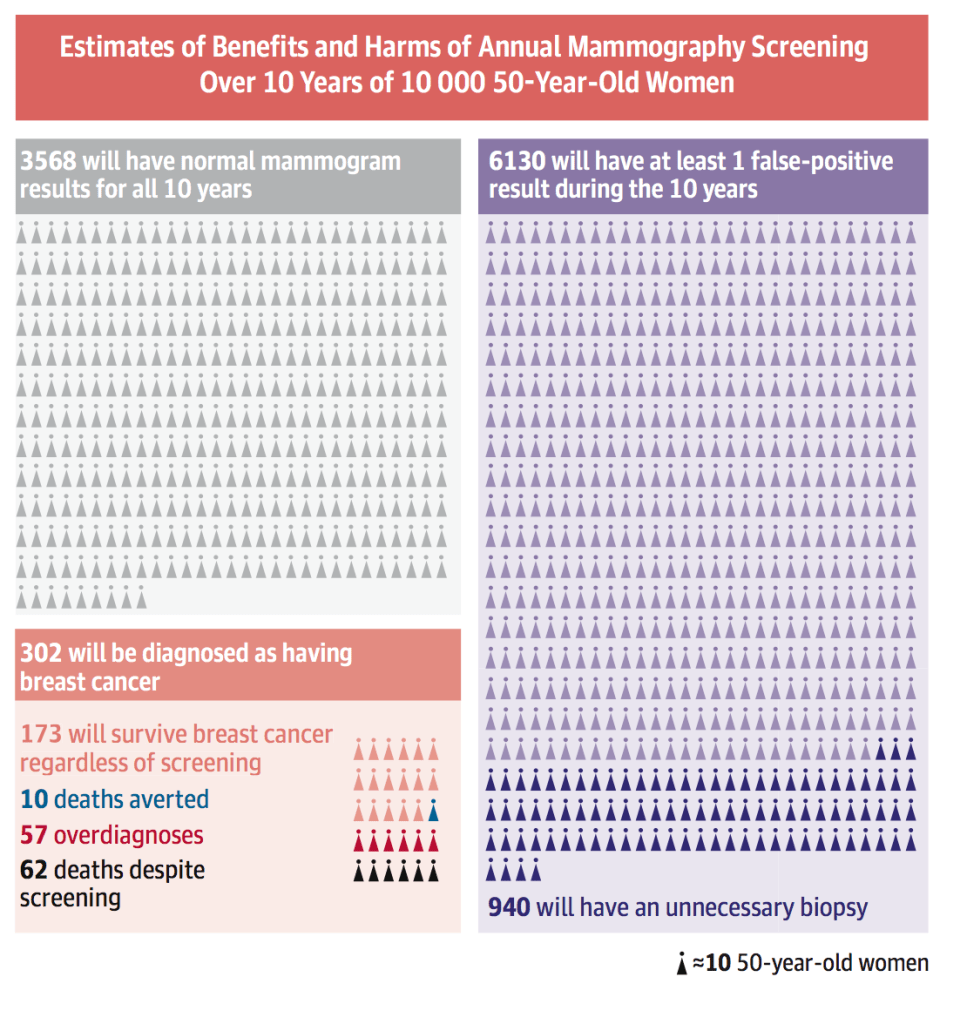
How many women are having discussions with their doctors about potential overdiagnosis of DCIS and a high chance of having an unnecessary biopsy?
Thankfully science writer Christie Aschwanden studied the issue and has written several articles on the topic in an effort to help women make informed choices. Her article, It’s Ok to Opt Out of Mammograms, is a must read!
Key points from article:
“The premise of screening is that it can find cancers destined to metastasize when they’re at an early stage so that they can be treated before they turn deadly. If this were the case, then finding and treating cancers at an early stage should reduce the rate at which cancers present at a later, metastatic stage. Unfortunately, that’s not what’s happened.”
Screening mammography has failed to reduce the incidence of metastatic disease and it’s created an epidemic of DCIS.
“…widespread mammography, able to detect smaller and smaller lesions, has led to a sevenfold increase in the number of new cases of DCIS. Today it accounts for about one in five breast cancer diagnoses, with some 64,000 women diagnosed with the condition last year.“
Mammography also leads to the treatment of cancers that never threatened the patient’s life, and these treatments can increase mortality.
There is also the serious issue of underdiagnosis.
Did you know –-Mammograms miss 40% of INVASIVE CANCER?!?!
What about Cumulative Radiation and Compression Harms?
This, too is controversial and a bit taboo to discuss, but it is a very real concern for many women. Doctors often dismiss any harm with statements like, “The amount of radiation is equivalent to flying across the US.”
There is a support group of over 250 women called Victims of Mammogram United.
Medical physicist John Gofman “argued forcefully that radiation is overused in medicine, both for diagnosis and treatment, without a full consideration of the risks.” Gofman and his colleague stated, “the risk from low doses of radiation was 20 times higher than stated by the government.” – LA TIMES 2007
He claimed, “There is NO safe dose of ionizing radiation.” More info here and here.
See chart here about radiation-induced breast cancers from mammography
More recent research about “Mammography-induced cancers” by Daniel Corcos is discussed in video here:
What opened my eyes in 2012?
A study published in the prestigious New England Journal of Medicine stated:
Results: …”we estimated that breast cancer was overdiagnosed (i.e., tumors were detected on screening that would never have led to clinical symptoms) in 1.3 million U.S. women in the past 30 years. We estimated that in 2008, breast cancer was overdiagnosed in more than 70,000 women; this accounted for 31% of all breast cancers diagnosed.
Conclusions: Despite substantial increases in the number of cases of early-stage breast cancer detected, screening mammography has only marginally reduced the rate at which women present with advanced cancer. Although it is not certain which women have been affected, the imbalance suggests that there is substantial overdiagnosis, accounting for nearly a third of all newly diagnosed breast cancers, and that screening is having, at best, only a small effect on the rate of death from breast cancer. – Effect of three decades of screening mammography on breast-cancer incidence
My investigation into overdiagnosis
Since 2012, I read and collected numerous articles and I wrote several blog posts. After many years, I created a page dedicated to this topic. Overdiagnosis 411
On a mammogram, a silent, indolent tumor looks the same as a deadly, progressive cancer that just hasn’t yet spread. If a clinician finds cancer on a mammogram, it often still triggers a slew of follow-up treatments possibly including biopsies, surgery, chemotherapy, and radiation — all unneeded and harmful interventions if the cancer was destined to remain silent.” – How often is breast cancer overdiagnosed? New research finds true cases far outweigh false alarms
Cancer Research UK states: Overdiagnosis: when finding cancer can do more harm than good
Overdiagnosis, in turn, leads to overtreatment, which is the treatment of clinically insignificant disease, essentially giving too much treatment without benefit to the patient. Treating a cancer that is not life-threatening leads to significant harm for women. Accepting the Swiss Medical Board estimates, that means one in five women who was told she had breast cancer after her mammogram received unnecessary treatment for cancer. The result is that tens of thousands of women in the U.S. each year are treated unnecessarily for breast cancer and undergo surgery, radiation and chemotherapy for tumors that are not and never would be life threatening. – How Routine Mammography Screening Leads to Overdiagnosis & Overtreatment, Breast Cancer Action
My investigation into another major harm from mammography screening…
Too Many Unnecessary Biopsies
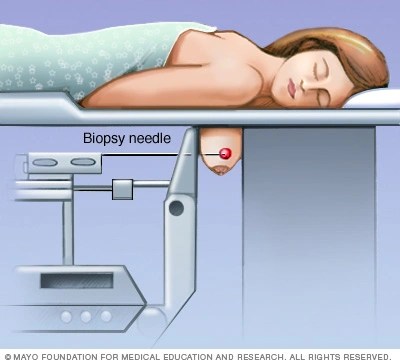
1.6 million breast biopsies are performed each year in the US, and approximately 80% are found to be benign.
One study found that false-positive mammograms and breast cancer over-diagnosis account for $4 billion dollars in spending every year.

ABC Investigates featured my story and the problem of overdiagnosis: Is Stage Zero breast cancer really cancer? 7 ON YOUR SIDE investigates the controversy
Women’s perceptions do not match scientific data.

Women may hear…
“Regular mammograms reduce breast cancer deaths by 20%.”
Sounds pretty good…but how many lives do they really save?
Only 1 in 1,000!
A short video explains in a simple way:
Are there safer, more accurate ways of monitoring breast health?
Please read:
Breast Imaging Options — A Patient Advocate Investigates ABUS and QT

Informed consent about mammography screening is important!
What is Informed Consent?
“Informed consent is the process in which a health care provider educates a patient about the risks, benefits, and alternatives of a given procedure or intervention. The patient must be competent to make a voluntary decision about whether to undergo the procedure or intervention. Informed consent is both an ethical and legal obligation of medical practitioners in the US and originates from the patient’s right to direct what happens to their body. Implicit in providing informed consent is an assessment of the patient’s understanding, rendering an actual recommendation, and documentation of the process. The Joint Commission requires documentation of all the elements of informed consent “in a form, progress notes or elsewhere in the record.” The following are the required elements for documentation of the informed consent discussion: (1) the nature of the procedure, (2) the risks and benefits and the procedure, (3) reasonable alternatives, (4) risks and benefits of alternatives, and (5) assessment of the patient’s understanding of elements 1 through 4.
It is the obligation of the provider to make it clear that the patient is participating in the decision-making process and avoid making the patient feel forced to agree to with the provider. The provider must make a recommendation and provide their reasoning for said recommendation.” – Informed Consent, https://www.ncbi.nlm.nih.gov/books/NBK430827/
PLEASE SIGN & SHARE PETITION:
INFORMED CHOICE in Breast Cancer Screening / Insurance for Ultrasound and QT Imaging
A wealth of information to understand all the potential harms of mammography can be found at:
